Pityriasis Versicolor in Adolescents: What You Should Know

Pityriasis versicolor is one of the most frequent reasons for dermatological consultation in adolescents. Although it’s a disease that’s neither serious nor has alarming symptoms, it usually affects the quality of life of those who suffer from it. Especially during the warmer months, when more of the body surface is exposed. Are you interested in learning more about this condition? Take note!
What is pityriasis versicolor in adolescents?
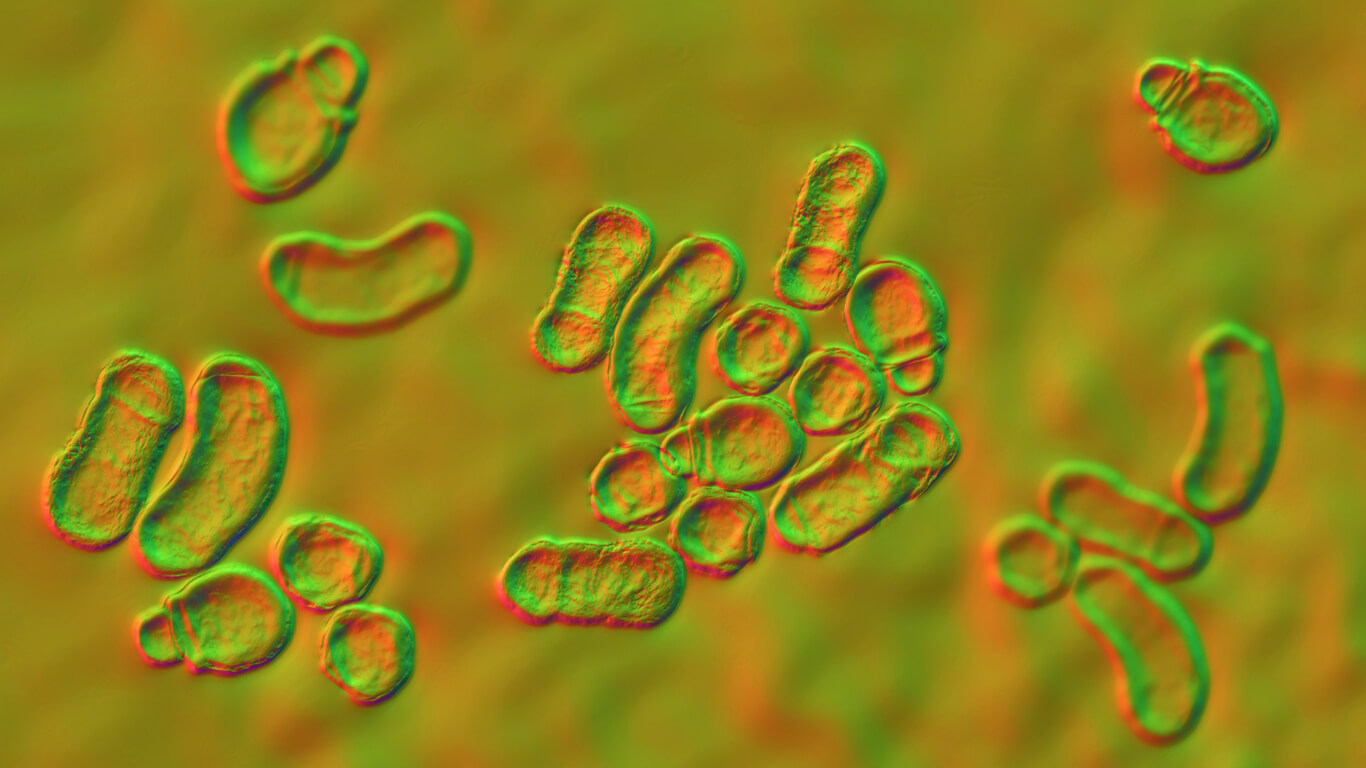
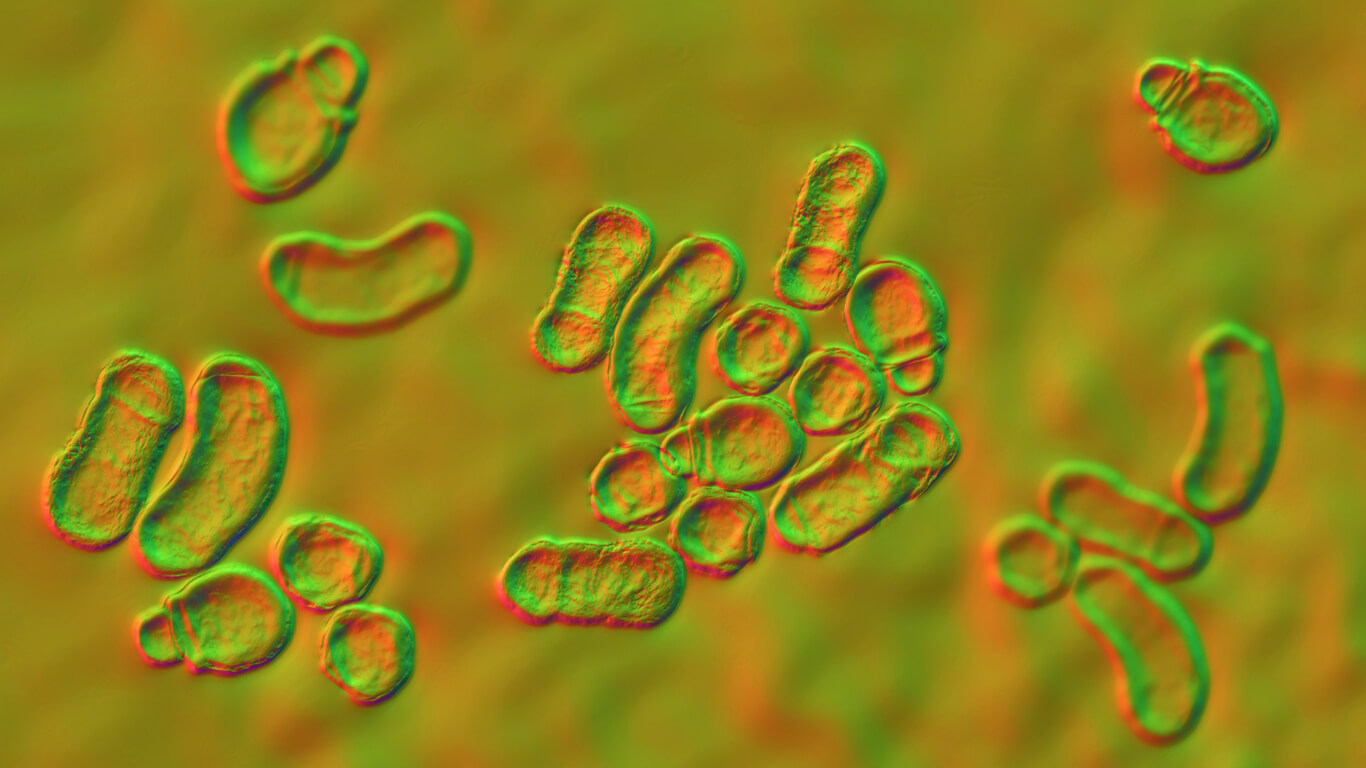
The Malassezia fungus is a variety of yeast that’s part of the skin’s microbiota. In general, it doesn’t usually cause any serious health problems and helps to protect us from pathogenic germs entering the body.
Under certain circumstances, this yeast can reproduce excessively and alter the health of the skin, especially its pigmentation. Then, there are more or less pigmented areas that modify the aesthetics of the tissue.
This condition isn’t contagious (because it’s a fungus that lives on our skin) and the pathology occurs when our immunity decreases. In other words, it’s an opportunistic infection.

Causes of pityriasis versicolor in adolescents
As mentioned above, uncontrolled growth of Malassezia on the skin surface leads to the development of pityriasis versicolor. Some of the predisposing factors are as follows:
- Excessive sweating
- Hot and humid climate
- Hormonal alterations
- A weakened immune system
- A family history of the pathology
- Skin with oily characteristics
While pityriasis Versicolor can occur in any ethnicity and age, it’s most common in adolescents and young adults.
You may be interested in: Pigmentation Disorders in Children: What You Should Know
Symptoms of pityriasis versicolor
Depigmented plaques on the skin surface are the most obvious sign of this condition and usually appear on the chest, arms, back, and neck. These macules may have the following characteristics:
- More or less pigment with respect to the surrounding skin (in general, they’re pink or red)
- Mild flaking
- Dryness (which favors itching)
- A tendency to improve in dry and cold climates
- Increased appearance with tanning
How is pityriasis versicolor diagnosed?
Whenever pigmentation changes appear on the skin, it’s important to consult a specialist physician. Ideally, don’t try to treat them with home treatments, as this could worsen the clinical picture.
The doctor will examine the skin surface and will determine if it’s pityriasis versicolor just by looking at the lesions. However, according to a publication of the American Academy of Dermatology Association, a skin scraping may be performed if necessary to corroborate the diagnosis. This gentle skin scraping removes epidermal cells so that they can be studied under a microscope.
On some occasions, the physician may take a biopsy, which is a sample of the affected tissue, for analysis. Even Wood’s lamp is very useful for this type of disease, as through observation with ultraviolet light at a distance of 4 to 5 inches, it’s possible to observe the fungus in green or yellow color.
Therapeutic options for pityriasis versicolor in adolescents
After diagnosis, the specialist will indicate different medications such as topical creams, which are the first line of treatment for this condition. Some of them include the following components:
- Non-specific antifungal agents: Sulfur plus salicylic acid, zinc pyrithione, and selenium sulfide 2.5%.
- Specific antifungal agents: Imidazoles (ketoconazole 2%, clotrimazole 1%, econazole, miconazole, isoconazole), allylamine (terbinafine 1%) and ciclopirox olamine 1%.
In turn, the physician may consider adding oral medication for the treatment of this disease. The most recommended are usually the following drugs:
- Fluconazole
- Ketoconazole
- Itraconazole
Spray or foaming lotion forms are preferable to creams, as the latter are more oily and more complicated to apply and distribute over large areas.
In addition, the patient should be informed that the agent causing the condition is a commensal fungus that makes up the microbiota of the skin. Therefore, this pathology isn’t considered contagious.
How long does it take for the clinical picture to resolve?
Once treatment is implemented, the prognosis improves in the long term, as even if the infection is eradicated, the skin may remain hypopigmented for several weeks.
Also, the condition may recur if the skin returns to humid or warm climates. However, the condition itself doesn’t cause pigmentary disorders or permanent scarring.
Read also: Medical Check-Ups During Adolescence
Pityriasis versicolor in adolescence and its appearance
As it’s a yeast that normally inhabits the skin, it should be considered a condition that tends to recur over time. Therefore, if it has already occurred on previous occasions, it’s best to take appropriate measures to prevent its recurrence.
Pityriasis versicolor is one of the most frequent reasons for dermatological consultation in adolescents. Although it’s a disease that’s neither serious nor has alarming symptoms, it usually affects the quality of life of those who suffer from it. Especially during the warmer months, when more of the body surface is exposed. Are you interested in learning more about this condition? Take note!
What is pityriasis versicolor in adolescents?
The Malassezia fungus is a variety of yeast that’s part of the skin’s microbiota. In general, it doesn’t usually cause any serious health problems and helps to protect us from pathogenic germs entering the body.
Under certain circumstances, this yeast can reproduce excessively and alter the health of the skin, especially its pigmentation. Then, there are more or less pigmented areas that modify the aesthetics of the tissue.
This condition isn’t contagious (because it’s a fungus that lives on our skin) and the pathology occurs when our immunity decreases. In other words, it’s an opportunistic infection.

Causes of pityriasis versicolor in adolescents
As mentioned above, uncontrolled growth of Malassezia on the skin surface leads to the development of pityriasis versicolor. Some of the predisposing factors are as follows:
- Excessive sweating
- Hot and humid climate
- Hormonal alterations
- A weakened immune system
- A family history of the pathology
- Skin with oily characteristics
While pityriasis Versicolor can occur in any ethnicity and age, it’s most common in adolescents and young adults.
You may be interested in: Pigmentation Disorders in Children: What You Should Know
Symptoms of pityriasis versicolor
Depigmented plaques on the skin surface are the most obvious sign of this condition and usually appear on the chest, arms, back, and neck. These macules may have the following characteristics:
- More or less pigment with respect to the surrounding skin (in general, they’re pink or red)
- Mild flaking
- Dryness (which favors itching)
- A tendency to improve in dry and cold climates
- Increased appearance with tanning
How is pityriasis versicolor diagnosed?
Whenever pigmentation changes appear on the skin, it’s important to consult a specialist physician. Ideally, don’t try to treat them with home treatments, as this could worsen the clinical picture.
The doctor will examine the skin surface and will determine if it’s pityriasis versicolor just by looking at the lesions. However, according to a publication of the American Academy of Dermatology Association, a skin scraping may be performed if necessary to corroborate the diagnosis. This gentle skin scraping removes epidermal cells so that they can be studied under a microscope.
On some occasions, the physician may take a biopsy, which is a sample of the affected tissue, for analysis. Even Wood’s lamp is very useful for this type of disease, as through observation with ultraviolet light at a distance of 4 to 5 inches, it’s possible to observe the fungus in green or yellow color.
Therapeutic options for pityriasis versicolor in adolescents
After diagnosis, the specialist will indicate different medications such as topical creams, which are the first line of treatment for this condition. Some of them include the following components:
- Non-specific antifungal agents: Sulfur plus salicylic acid, zinc pyrithione, and selenium sulfide 2.5%.
- Specific antifungal agents: Imidazoles (ketoconazole 2%, clotrimazole 1%, econazole, miconazole, isoconazole), allylamine (terbinafine 1%) and ciclopirox olamine 1%.
In turn, the physician may consider adding oral medication for the treatment of this disease. The most recommended are usually the following drugs:
- Fluconazole
- Ketoconazole
- Itraconazole
Spray or foaming lotion forms are preferable to creams, as the latter are more oily and more complicated to apply and distribute over large areas.
In addition, the patient should be informed that the agent causing the condition is a commensal fungus that makes up the microbiota of the skin. Therefore, this pathology isn’t considered contagious.
How long does it take for the clinical picture to resolve?
Once treatment is implemented, the prognosis improves in the long term, as even if the infection is eradicated, the skin may remain hypopigmented for several weeks.
Also, the condition may recur if the skin returns to humid or warm climates. However, the condition itself doesn’t cause pigmentary disorders or permanent scarring.
Read also: Medical Check-Ups During Adolescence
Pityriasis versicolor in adolescence and its appearance
As it’s a yeast that normally inhabits the skin, it should be considered a condition that tends to recur over time. Therefore, if it has already occurred on previous occasions, it’s best to take appropriate measures to prevent its recurrence.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Cogen AL, Nizet V, Gallo RL. Skin microbiota: a source of disease or defence?. Br J Dermatol. 2008;158(3):442-455. doi:10.1111/j.1365-2133.2008.08437.x
- Tinea versicolor: Diagnosis and treatment. [Internet] Disponible en: https://www.aad.org/public/diseases/a-z/tinea-versicolor-treatment
- Karray M, McKinney WP. Tinea Versicolor. 2021 Aug 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29494106.
-
Karray M, McKinney WP. Tinea Versicolor. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482500/
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








