Hope for Childhood Leukemia: Gene Therapy


Written and verified by the biologist Olga Carbajo
The most recent treatments against one of the most common cancers among children haven’t only managed to keep the illness from spreading, but they’ve also been able to reverse it. Gene therapy is giving those who suffer from B-cell childhood leukemia a new chance at life.
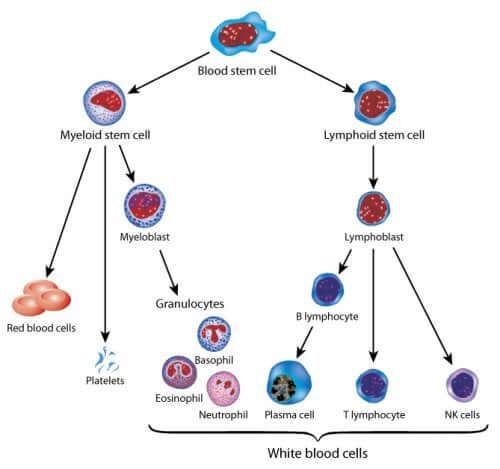
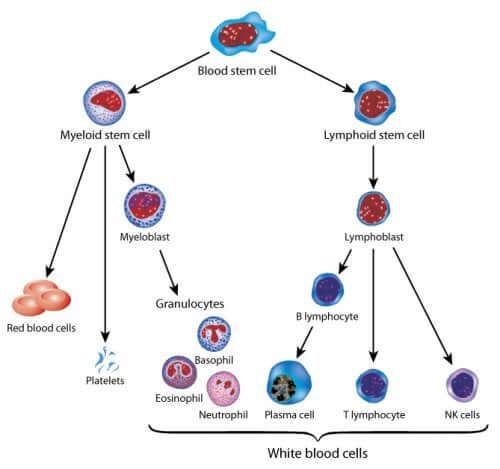
In order to understand leukemia, we first need to understand the cells it affects and how it develops. It all starts in bone marrow, a spongy tissue that is white in color. It’s located in the interior of large bones like the femur, hip and sternum.
Bone marrow contains a reduced number of stem cells that give birth to the types of cells we find in blood. These include lymphoid stem cells (lymphocytes) and myeloid stem cells (red blood cells, plachets and some white blood cells). So then, how does B-cell cancer start?
What is childhood leukemia?
Every form of cancer begins when our bodies start to produce cells and at an uncontrolled rate. These abnormal cells are unique in that they don’t die. Given that our bodies are made up of cells, cancer can appear in any of our organs.
In the case of childhood leukemia, the cancer originates in the bone marrow, meaning it affects the blood cells. In particular, it affects those that produce white blood cells and myeloid cells, myelocytes.
These cancerous cells, on occasion, remain in the bone marrow. However, they generally get into the bloodstream, thus spreading the illness. In some cases, the cancer invades other parts of the body. For example, lymphatic glands, the spleen, the liver and the central nervous system.
Types of childhood leukemia
According to various characteristics, The American Cancer Society classifies childhood leukemia into several different subtypes. These are: acute or fast growing, chronic or slower growing, involving myeloid cells or lymphoid cells.
- Acute lymphocytic leukemia (ALL). This is the most common type of childhood leukemia, involving the formation of white blood cells. It’s known as B-cell leukemia.
- Acute myeloid leukemia (AML). This cancer originates in the myeloid cells. It represents the majority of cases of residual leukemia.
- Chronic lymphocytic Leukemia (CLL). This type of leukemia is infrequent in children. It affects the white blood cells of the bone marrow.
- Chronic Myeloid Leukemia (CML). This variation originates in haematopoietic cells, which produce red blood cells and plackets, invading the bloodstream. It’s uncommon in children.
A ray of hope: Gene therapy
Recently, the Clinic of Barcelona, Spain treated several children with B-cell LLA who weren’t responding to conventional treatment. They applied new gene therapy – tisagenlecleucel – which is still in its experimental phase in humans.
This treatment was approved in 2012 by the FDA and is distributed by the pharmaceutical company Novartis. But, what exactly does gene therapy consist of?
Gene therapy
Gene therapy is a treatment that adjusts to each patient. It consists of introducing specific genes into the patient’s cells in order to combat the illness. This way, they avoid possible transplant rejections and increase the effectiveness of treatment by designing specific target cells for attacking cancer.
Designing the treatment of childhood leukemia
The process consists of several steps and lasts 22 days until completion.
- First of all, specialists extract blood cells from the patient and isolate the T lymphocytes.
- Next, in a laboratory, they manipulate these cells genetically. They give them a DNA sequence in order to produce a protein called CAR (Chimeric Antigen Receptor).
- The Chimeric Antigen Receptor is responsible for recognizing another protein located in the surface of the cancerous cells, la CD19.
- The patient’s T lymphocytes (TL) that have undergone genetic modification continue to grow in the lab until there are billions of them.
- In the final phase, the modified T lymphocytes are given to the patient in the form of an intravenous catheter.
How does the T-CAR/CD19 binomial work?
Imagine the cell like a sphere whose surface is flourishing with stick-like structures. Each of these structures has its own morphological characteristics. These sticks are responsible for the relationship between the cell and its surroundings, and with other cells.
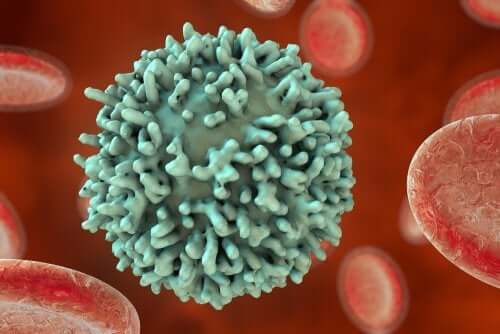
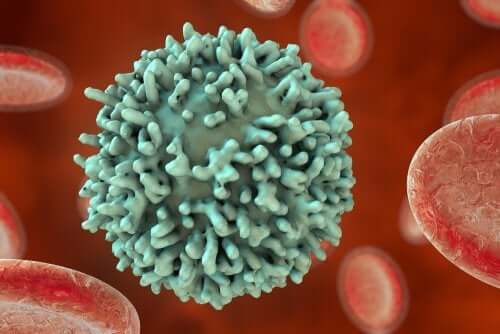
In the case of childhood leukemia, the person’s modified TL have a very concrete stick structure on their surface. The CAR specifically recognize another stick structure on the surface of the LB, the CD10. Now that the T lymphocyte has recognized the cancerous B cell, it can proceed with its elimination.
However, as Dr. Francis Collins, director of the National Institutes of Health stated, there are many issues to take into account before proclaiming the success of cancer immunotherapies as an unconditional success.
“We have seen dramatic responses from immunotherapy… We need to bring that kind of success—and hope—for more people and more types of cancer, and we need to do it quickly.”– Dr. Francis Collins –
Successes and failures of immunotherapy in childhood cancer
In the results observed over three months of the treatment application, 80% of patients presented clear remission from the illness. These are all patients whose cancer didn’t respond favorably to conventional chemotherapy. The data comes from the National Cancer Institute.
However, we need to be careful when it comes to the success of immunotherapy. This is in sight of the side effects observed, which experts cannot ignore. Dr.Collins presented a report regarding this issue, highlighting the following points:
- The CD19 protein is present in B lymphocytes, so LT-CDR doesn’t differentiate between cancerous cells and healthy cells. Thus, patients need to undergo treatment for immunosuppression.
- The appearance of cytokine release syndrome, which occurs through the application of the medication.
- The presence of neurological side effects, like confusion and convulsion. These side effects seem to go away without the need for treatment.
Of course, this innovative treatment represents a new ray of hope for families whose children suffer from cancer. Scientists are still perfecting the treatment, and it’s still in an experimental stage.
Just the same, the results have been positive, to say the least, when it comes to immunotherapy for other cancers as well, like HPV and lymphoma.
The most recent treatments against one of the most common cancers among children haven’t only managed to keep the illness from spreading, but they’ve also been able to reverse it. Gene therapy is giving those who suffer from B-cell childhood leukemia a new chance at life.
In order to understand leukemia, we first need to understand the cells it affects and how it develops. It all starts in bone marrow, a spongy tissue that is white in color. It’s located in the interior of large bones like the femur, hip and sternum.
Bone marrow contains a reduced number of stem cells that give birth to the types of cells we find in blood. These include lymphoid stem cells (lymphocytes) and myeloid stem cells (red blood cells, plachets and some white blood cells). So then, how does B-cell cancer start?
What is childhood leukemia?
Every form of cancer begins when our bodies start to produce cells and at an uncontrolled rate. These abnormal cells are unique in that they don’t die. Given that our bodies are made up of cells, cancer can appear in any of our organs.
In the case of childhood leukemia, the cancer originates in the bone marrow, meaning it affects the blood cells. In particular, it affects those that produce white blood cells and myeloid cells, myelocytes.
These cancerous cells, on occasion, remain in the bone marrow. However, they generally get into the bloodstream, thus spreading the illness. In some cases, the cancer invades other parts of the body. For example, lymphatic glands, the spleen, the liver and the central nervous system.
Types of childhood leukemia
According to various characteristics, The American Cancer Society classifies childhood leukemia into several different subtypes. These are: acute or fast growing, chronic or slower growing, involving myeloid cells or lymphoid cells.
- Acute lymphocytic leukemia (ALL). This is the most common type of childhood leukemia, involving the formation of white blood cells. It’s known as B-cell leukemia.
- Acute myeloid leukemia (AML). This cancer originates in the myeloid cells. It represents the majority of cases of residual leukemia.
- Chronic lymphocytic Leukemia (CLL). This type of leukemia is infrequent in children. It affects the white blood cells of the bone marrow.
- Chronic Myeloid Leukemia (CML). This variation originates in haematopoietic cells, which produce red blood cells and plackets, invading the bloodstream. It’s uncommon in children.
A ray of hope: Gene therapy
Recently, the Clinic of Barcelona, Spain treated several children with B-cell LLA who weren’t responding to conventional treatment. They applied new gene therapy – tisagenlecleucel – which is still in its experimental phase in humans.
This treatment was approved in 2012 by the FDA and is distributed by the pharmaceutical company Novartis. But, what exactly does gene therapy consist of?
Gene therapy
Gene therapy is a treatment that adjusts to each patient. It consists of introducing specific genes into the patient’s cells in order to combat the illness. This way, they avoid possible transplant rejections and increase the effectiveness of treatment by designing specific target cells for attacking cancer.
Designing the treatment of childhood leukemia
The process consists of several steps and lasts 22 days until completion.
- First of all, specialists extract blood cells from the patient and isolate the T lymphocytes.
- Next, in a laboratory, they manipulate these cells genetically. They give them a DNA sequence in order to produce a protein called CAR (Chimeric Antigen Receptor).
- The Chimeric Antigen Receptor is responsible for recognizing another protein located in the surface of the cancerous cells, la CD19.
- The patient’s T lymphocytes (TL) that have undergone genetic modification continue to grow in the lab until there are billions of them.
- In the final phase, the modified T lymphocytes are given to the patient in the form of an intravenous catheter.
How does the T-CAR/CD19 binomial work?
Imagine the cell like a sphere whose surface is flourishing with stick-like structures. Each of these structures has its own morphological characteristics. These sticks are responsible for the relationship between the cell and its surroundings, and with other cells.
In the case of childhood leukemia, the person’s modified TL have a very concrete stick structure on their surface. The CAR specifically recognize another stick structure on the surface of the LB, the CD10. Now that the T lymphocyte has recognized the cancerous B cell, it can proceed with its elimination.
However, as Dr. Francis Collins, director of the National Institutes of Health stated, there are many issues to take into account before proclaiming the success of cancer immunotherapies as an unconditional success.
“We have seen dramatic responses from immunotherapy… We need to bring that kind of success—and hope—for more people and more types of cancer, and we need to do it quickly.”– Dr. Francis Collins –
Successes and failures of immunotherapy in childhood cancer
In the results observed over three months of the treatment application, 80% of patients presented clear remission from the illness. These are all patients whose cancer didn’t respond favorably to conventional chemotherapy. The data comes from the National Cancer Institute.
However, we need to be careful when it comes to the success of immunotherapy. This is in sight of the side effects observed, which experts cannot ignore. Dr.Collins presented a report regarding this issue, highlighting the following points:
- The CD19 protein is present in B lymphocytes, so LT-CDR doesn’t differentiate between cancerous cells and healthy cells. Thus, patients need to undergo treatment for immunosuppression.
- The appearance of cytokine release syndrome, which occurs through the application of the medication.
- The presence of neurological side effects, like confusion and convulsion. These side effects seem to go away without the need for treatment.
Of course, this innovative treatment represents a new ray of hope for families whose children suffer from cancer. Scientists are still perfecting the treatment, and it’s still in an experimental stage.
Just the same, the results have been positive, to say the least, when it comes to immunotherapy for other cancers as well, like HPV and lymphoma.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- NIH. (19 octubre 2017). La terapia con células T y CAR ha sido aprobada para algunos niños y adultos jóvenes con leucemia [artículo en web]. Recuperado de: www.cancer.gov
- Mouzzo, J. (28 noviembre 2017). La terapia génica contra la leucemia llega al Clinic [artículo en periódico]. Recuperado de: www.elpais.com
- American Cancer Society. (12 febrero 2019). Tasa de supervivencia de las leucemias en niños [artículo en web]. Recuperado de: www.cancer.org
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








