The Importance of the Microbiome During Pregnancy and Lactation

The term “microbiome” has revolutionized the way we view the microbes inside and outside our bodies. Especially because of the knowledge that it’s inherited from the womb and, at birth, is enhanced by breastfeeding. But why is the importance of the microbiome during pregnancy and lactation? Among other reasons, the set of microorganisms exchanged between the baby and the mother affects the state of health of both. Keep reading to learn more about this topic.
Today, experts consider the microbiome to be one more organ of the body. Moreover, its colonization depends on several factors, such as nutrition and stage of growth. For example, a breastfed newborn will have different bacteria than a formula-fed infant.
How to differentiate microbiome from microbiota?
Although microbial communities have evolved along with science, there are still misunderstandings when talking about microbiomes or microbiota. They are even sometimes used as synonyms.
Microbiota
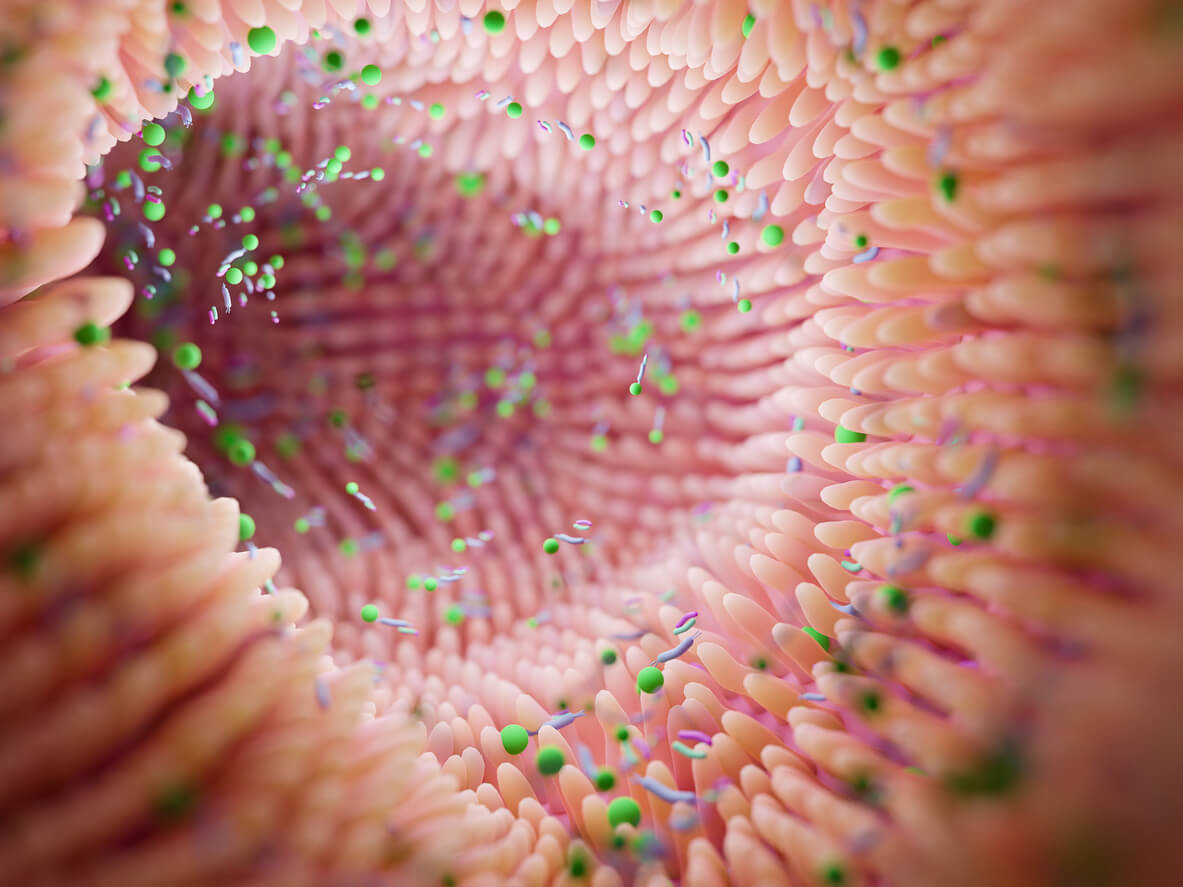
The first thing to know is that our entire body is colonized by trillions of microorganisms (bacteria, viruses, fungi, and others). These form communities in different organs, such as the skin, vagina, mouth, urinary tract, and intestine, among others.
The Spanish Journal of Digestive Diseases, in 2018, clarified that those communities of microorganisms that reside in a specific site of the body are called microbiota. Therefore, we find one that inhabits the skin, one that inhabits the intestines–known as intestinal flora–and one that inhabits the mouth, among others. The interesting thing is that each of them has its own characteristics.
Microbiome
On the other hand, the microbiome considers all the communities of microorganisms, as well as their genes and the metabolites they form. It varies for each person and colonization occurs throughout life. It can be said that the microbiome is like a fingerprint, as it’s unique to each of us.
You can also read: 4 Tips for Taking Care of Your Children’s Microbiota
The importance of the microbiome during pregnancy and lactation
During pregnancy and lactation, hormonal, immune, and metabolic changes occur that particularly modify the intestinal microbiota. This has a high impact on the health of the mother-child binomial. As stated by some authors in the journal Infection and Gut Resistance, the changes during pregnancy are related to the modification in the composition of the intestine and its diversity.
Benefits for the mother
The journal Nature explains that trimestral changes in the intestinal microflora occur during pregnancy. These modifications affect the immunity, metabolism, digestion, and neurological development of the pregnant woman and her baby. Likewise, an imbalance of the microflora is associated with certain chronic diseases such as diabetes, hypertension, and inflammatory bowel disease.
It’s also important to take into account that changes in the intestinal flora are affected by genetics, certain environmental factors, and the dietary habits of the pregnant woman. This was reported by a group of researchers in the journal Nature in 2018.
Benefits for the baby
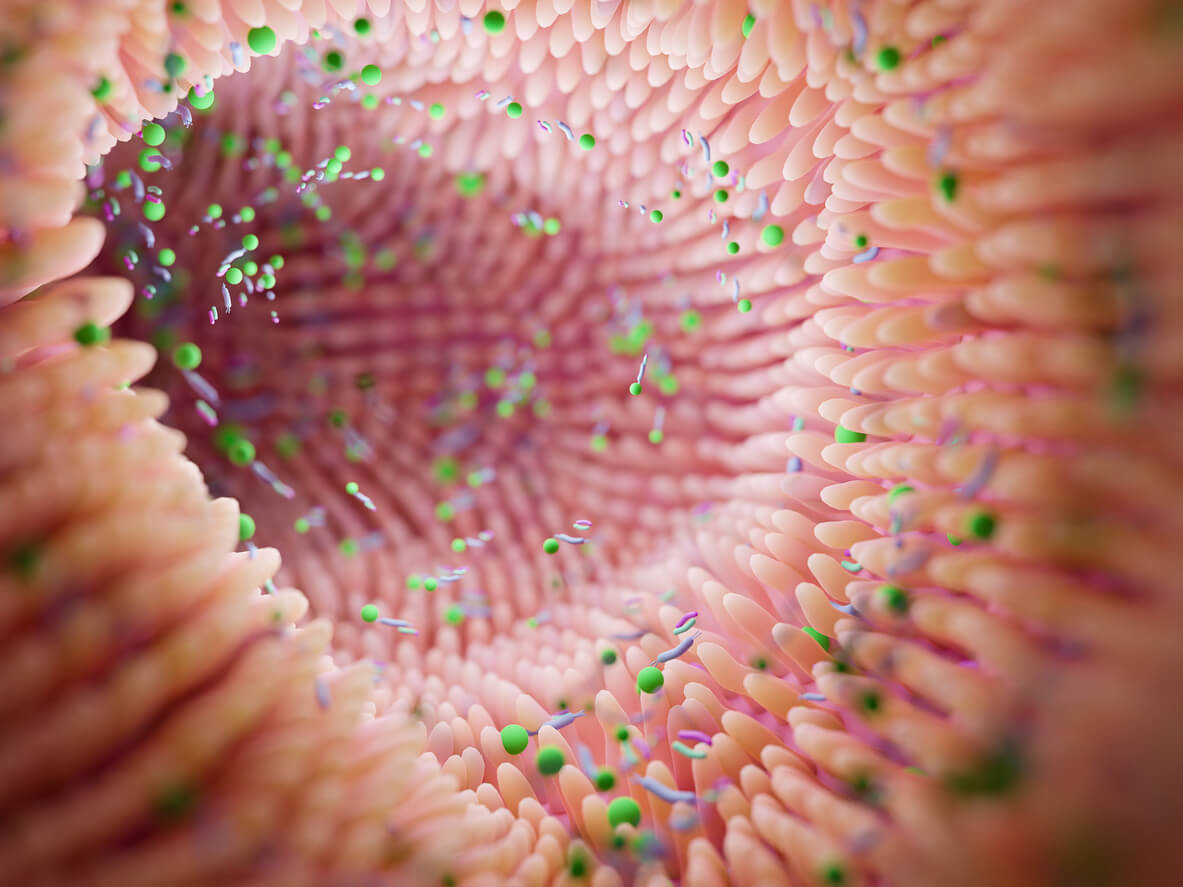
As we read in an analysis published in the journal Life, there are several ways to colonize the baby’s gut during its stay in the womb. For example, through direct transmission from the mother’s womb to the child.
The mode of birth also affects the variety of the child’s intestinal microflora. In addition, the diversity is greater in vaginal births than in cesarean deliveries. Gestational age also plays a role. For example, there are fewer beneficial bacteria in preterm babies.
Therefore, a baby’s immune system begins to form before birth to deal with possible harmful bacteria. In this regard, an article on the Only About Children website mentions that 70% of the baby’s immune system is located in the intestine. In addition, this microbiota helps improve digestion and nutrient absorption and stimulates the production of neurotransmitters that control feelings of fear and anxiety.
The benefits of breastfeeding for the microbiome
Colonization of the baby’s gut bacteria doesn’t only occur in the womb. At birth, breast milk increases their biodiversity. Some scientific data highlight the presence of lactobacilli and bifidobacteria in the food, which increases the intestinal microbiota by 85% with health benefits. These are known as probiotics.
An article published by the University Isabel I in 2022 explains that milk also contains special carbohydrates known as prebiotics. A review of articles shared by the journal Nutrients, in 2020, makes it clear that they benefit the maturation and development of the immune system, as well as the integrity of the intestinal mucosa and the production of IgA antibodies.
In addition, as detailed in a review in the journal Pediatrics, probiotics also reduce the risk of obesity, diabetes, hypertension, and increased blood cholesterol in infants and in adulthood. These are some reasons why health agencies recommend exclusive breastfeeding until the first 6 months of age.
Read also: The Relationship Between Breastfeeding and a Baby’s Immune System

What should the diet of pregnant and breastfeeding women be like?
As a study in the journal Gut Microbes reveals, maternal nutrition during pregnancy and lactation has an impact on the abundance and prevalence of the gut microbiota.
What to include and what not to include in the diet
Some recommendations for a diet that promotes the growth of beneficial bacteria for the health of mother and baby are as follows:
- Increase the consumption of prebiotic fiber, as indicated in the Journal of Food Science and Technology. Good options are the fructooligosaccharides found in banana, onion, asparagus, strawberries, apple, or chicory, among others. In addition, fiber from whole grains, vegetables, and legumes also provides nutrients for the intestinal microbiota of the colon.
- Include more probiotic foods suitable for pregnancy, such as yogurt, tempeh, water kefir, and sauerkraut, among others.
- Increase omega-3 and omega-9 fats. This can be achieved by including sardines, mackerel, bonito, salmon, and tuna in the diet. In turn, olive oil should prevail.
- Increase the portion of fruits between 4 and 5 times a day.
- Maintain a diet low in saturated and trans fats and ultra-processed foods, such as sugars, desserts, pastries, cakes, chips, donuts, and fast foods.
- Follow a healthy diet, indicated and guided by health professionals during pregnancy.
What we must do to maintain a healthy microbiome during pregnancy and breastfeeding
There’s no doubt that the microbiome is part of our lives and that it’s especially important during pregnancy and breastfeeding. And to shape it from an early age, we depend on a healthy pregnancy and exclusive breastfeeding for the first 6 months of life.
A healthy microbiome benefits not only the mother’s health but also that of the baby. It also increases the body’s defenses and reduces the risk of certain chronic diseases in adulthood, among other benefits.
A healthy pregnancy depends on a good diet, including nutrients that strengthen the intestinal microbiota. In this regard, prebiotic fiber should be included, such as oligosaccharides contained in vegetables, fruits, and legumes. In addition, whole grains and their derivatives should also be taken into account.
The term “microbiome” has revolutionized the way we view the microbes inside and outside our bodies. Especially because of the knowledge that it’s inherited from the womb and, at birth, is enhanced by breastfeeding. But why is the importance of the microbiome during pregnancy and lactation? Among other reasons, the set of microorganisms exchanged between the baby and the mother affects the state of health of both. Keep reading to learn more about this topic.
Today, experts consider the microbiome to be one more organ of the body. Moreover, its colonization depends on several factors, such as nutrition and stage of growth. For example, a breastfed newborn will have different bacteria than a formula-fed infant.
How to differentiate microbiome from microbiota?
Although microbial communities have evolved along with science, there are still misunderstandings when talking about microbiomes or microbiota. They are even sometimes used as synonyms.
Microbiota
The first thing to know is that our entire body is colonized by trillions of microorganisms (bacteria, viruses, fungi, and others). These form communities in different organs, such as the skin, vagina, mouth, urinary tract, and intestine, among others.
The Spanish Journal of Digestive Diseases, in 2018, clarified that those communities of microorganisms that reside in a specific site of the body are called microbiota. Therefore, we find one that inhabits the skin, one that inhabits the intestines–known as intestinal flora–and one that inhabits the mouth, among others. The interesting thing is that each of them has its own characteristics.
Microbiome
On the other hand, the microbiome considers all the communities of microorganisms, as well as their genes and the metabolites they form. It varies for each person and colonization occurs throughout life. It can be said that the microbiome is like a fingerprint, as it’s unique to each of us.
You can also read: 4 Tips for Taking Care of Your Children’s Microbiota
The importance of the microbiome during pregnancy and lactation
During pregnancy and lactation, hormonal, immune, and metabolic changes occur that particularly modify the intestinal microbiota. This has a high impact on the health of the mother-child binomial. As stated by some authors in the journal Infection and Gut Resistance, the changes during pregnancy are related to the modification in the composition of the intestine and its diversity.
Benefits for the mother
The journal Nature explains that trimestral changes in the intestinal microflora occur during pregnancy. These modifications affect the immunity, metabolism, digestion, and neurological development of the pregnant woman and her baby. Likewise, an imbalance of the microflora is associated with certain chronic diseases such as diabetes, hypertension, and inflammatory bowel disease.
It’s also important to take into account that changes in the intestinal flora are affected by genetics, certain environmental factors, and the dietary habits of the pregnant woman. This was reported by a group of researchers in the journal Nature in 2018.
Benefits for the baby
As we read in an analysis published in the journal Life, there are several ways to colonize the baby’s gut during its stay in the womb. For example, through direct transmission from the mother’s womb to the child.
The mode of birth also affects the variety of the child’s intestinal microflora. In addition, the diversity is greater in vaginal births than in cesarean deliveries. Gestational age also plays a role. For example, there are fewer beneficial bacteria in preterm babies.
Therefore, a baby’s immune system begins to form before birth to deal with possible harmful bacteria. In this regard, an article on the Only About Children website mentions that 70% of the baby’s immune system is located in the intestine. In addition, this microbiota helps improve digestion and nutrient absorption and stimulates the production of neurotransmitters that control feelings of fear and anxiety.
The benefits of breastfeeding for the microbiome
Colonization of the baby’s gut bacteria doesn’t only occur in the womb. At birth, breast milk increases their biodiversity. Some scientific data highlight the presence of lactobacilli and bifidobacteria in the food, which increases the intestinal microbiota by 85% with health benefits. These are known as probiotics.
An article published by the University Isabel I in 2022 explains that milk also contains special carbohydrates known as prebiotics. A review of articles shared by the journal Nutrients, in 2020, makes it clear that they benefit the maturation and development of the immune system, as well as the integrity of the intestinal mucosa and the production of IgA antibodies.
In addition, as detailed in a review in the journal Pediatrics, probiotics also reduce the risk of obesity, diabetes, hypertension, and increased blood cholesterol in infants and in adulthood. These are some reasons why health agencies recommend exclusive breastfeeding until the first 6 months of age.
Read also: The Relationship Between Breastfeeding and a Baby’s Immune System

What should the diet of pregnant and breastfeeding women be like?
As a study in the journal Gut Microbes reveals, maternal nutrition during pregnancy and lactation has an impact on the abundance and prevalence of the gut microbiota.
What to include and what not to include in the diet
Some recommendations for a diet that promotes the growth of beneficial bacteria for the health of mother and baby are as follows:
- Increase the consumption of prebiotic fiber, as indicated in the Journal of Food Science and Technology. Good options are the fructooligosaccharides found in banana, onion, asparagus, strawberries, apple, or chicory, among others. In addition, fiber from whole grains, vegetables, and legumes also provides nutrients for the intestinal microbiota of the colon.
- Include more probiotic foods suitable for pregnancy, such as yogurt, tempeh, water kefir, and sauerkraut, among others.
- Increase omega-3 and omega-9 fats. This can be achieved by including sardines, mackerel, bonito, salmon, and tuna in the diet. In turn, olive oil should prevail.
- Increase the portion of fruits between 4 and 5 times a day.
- Maintain a diet low in saturated and trans fats and ultra-processed foods, such as sugars, desserts, pastries, cakes, chips, donuts, and fast foods.
- Follow a healthy diet, indicated and guided by health professionals during pregnancy.
What we must do to maintain a healthy microbiome during pregnancy and breastfeeding
There’s no doubt that the microbiome is part of our lives and that it’s especially important during pregnancy and breastfeeding. And to shape it from an early age, we depend on a healthy pregnancy and exclusive breastfeeding for the first 6 months of life.
A healthy microbiome benefits not only the mother’s health but also that of the baby. It also increases the body’s defenses and reduces the risk of certain chronic diseases in adulthood, among other benefits.
A healthy pregnancy depends on a good diet, including nutrients that strengthen the intestinal microbiota. In this regard, prebiotic fiber should be included, such as oligosaccharides contained in vegetables, fruits, and legumes. In addition, whole grains and their derivatives should also be taken into account.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Chu, D. M., Meyer, K. M., Prince, A. L., & Aagaard, K. M. (2016). Impact of maternal nutrition in pregnancy and lactation on offspring gut microbial composition and function. Gut microbes, 7(6), 4 Pandey, K. R., Naik, S. R., & Vakil, B. V. (2015). Probiotics, prebiotics and synbiotics- a review. Journal of food science and technology, 52(12), 7577–7587. https://doi.org/10.1007/s13197-015-1921-159–470. https://doi.org/10.1080/19490976.2016.1241357
- Khan, I., Yasir, M., Farman, M., Kumosani, T., AlBasri, S. F., Bajouh, O. S., & Azhar, E. I. (2019). Evaluation of gut bacterial community composition and antimicrobial resistome in pregnant and non-pregnant women from Saudi population. Infection and drug resistance, 12, 1749–1761. https://doi.org/10.2147/IDR.S200213
- Łubiech, K., & Twarużek, M. (2020). Lactobacillus Bacteria in Breast Milk. Nutrients, 12(12), 3783. https://doi.org/10.3390/nu12123783
- Miko E, Csaszar A, Bodis J, Kovacs K. (2022). The Maternal–Fetal Gut Microbiota Axis: Physiological Changes, Dietary Influence, and Modulation Possibilities. Life. 12(3):424. https://doi.org/10.3390/life12030424
- Only About Children. (2023). The Importance of Good Gut Health in Children. Disponible en: https://www.oac.edu.au/news-views/the-importance-of-good-gut-health-in-children/#:~:text=Research%20suggests%20that%20a%20poor,children%20feeling%20energetic%20and%20healthy.
- Osorio L,, Umbarila A. (2015). Microbiota de la glándula mamaria. Vol 48, 1, 1-8. Disponible en: https://www.elsevier.es/es-revista-pediatria-213-articulo-microbiota-glandula-mamaria-S0120491215000026#:~:text=La%20microbiota%20de%20la%20gl%C3%A1ndula%20mamaria%20est%C3%A1%20formada%20por%20bacterias,los%20ni%C3%B1os%20que%20son%20amamantados.
- Pedersen, H. K., Gudmundsdottir, V., Nielsen, H. B., Hyotylainen, T., Nielsen, T., Jensen, B. A., Forslund, K., Hildebrand, F., Prifti, E., Falony, G., Le Chatelier, E., Levenez, F., Doré, J., Mattila, I., Plichta, D. R., Pöhö, P., Hellgren, L. I., Arumugam, M., Sunagawa, S., Vieira-Silva, S., … Pedersen, O. (2016). Human gut microbes impact host serum metabolome and insulin sensitivity. Nature, 535(7612), 376–381. https://doi.org/10.1038/nature18646
- Rothschild, D., Weissbrod, O., Barkan, E., Kurilshikov, A., Korem, T., Zeevi, D., Costea, P. I., Godneva, A., Kalka, I. N., Bar, N., Shilo, S., Lador, D., Vila, A. V., Zmora, N., Pevsner-Fischer, M., Israeli, D., Kosower, N., Malka, G., Wolf, B. C., Avnit-Sagi, T., … Segal, E. (2018). Environment dominates over host genetics in shaping human gut microbiota. Nature, 555(7695), 210–215. https://doi.org/10.1038/nature25973
- Sebastián-Domingo, Juan-J., & Sánchez-Sánchez, Clara. (2018). De la flora intestinal al microbioma. Revista Española de Enfermedades Digestivas, 110(1), 51-56. https://dx.doi.org/10.17235/reed.2017.4947/2017
- Section on Breastfeeding (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. https://doi.org/10.1542/peds.2011-3552
- Universidad Isabel I (2022). Campus Burgus. Lctancia materna y microbioma. Disponible en: https://www.ui1.es/blog-ui1/lactancia-materna-y-microbioma
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








