9 Questions About In Vitro Fertilization

Since the 1970s, the conception of a child outside the womb has been a reality. In fact, its frequency is such that we’ve already lost sight of the magnitude of the astonishing discovery of Robert Edwards and his colleagues. Today, millions of children come to the world thanks to advances in reproductive medicine. It’s estimated that between 1 and 3% of live births in Europe and the United States were conceived by in vitro fertilization (IVF). The dream of being a parent can come true and that’s why today, we want to answer the 9 most frequently asked questions about in vitro fertilization!
In vitro fertilization, 40 years fulfilling dreams
In 1978, Louise Brown, the first “test-tube baby”, conceived in the laboratory by IVF, came to this world. From there, for many families, the story began to change and their dream of being parents came true.
We know that any promising alternative brings with it fears and doubts, and that’s why we’re going to answer the most frequent questions about in vitro fertilization that arise among families. With information, it’s possible to make more conscious and wise decisions.

1. What is the in vitro fertilization technique?
IVF is a highly complex assisted fertilization (AF) technique, which specifies three fundamental steps of reproduction :
- Obtaining the mature oocyte (maternal gamete), from the aspiration of the pre-ovulatory follicle of the woman’s ovary.
- The fertilization of the oocyte by the sperm (paternal gamete): this gives rise to the egg or embryo.
- The transfer of the embryo into the uterine cavity, to complete its gestation.
This way, reproductive medicine specialists are in charge of executing a key step for the creation of life when it’s not possible to do it naturally.
2. When should couples consider this option?
AF techniques, especially IVF, are effective alternatives to conceiving a baby in those cases where there are difficulties in achieving it. And these can be medical issues, such as infertility, or social issues, such as single-parent families.
The most important thing is to consult a specialist in assisted reproduction so that they can evaluate each case in particular and suggest the most appropriate method.
3. How likely is this technique to be successful?
In general, the chances of conceiving naturally are around 20% in a young, healthy couple. But in medicine, the question isn’t mathematical. In fact, with successive attempts, this percentage drops month by month.
In the case of IVF, the success rate depends on many factors, including maternal age. According to data from the National Institute of Health and Care Excellence in the United Kingdom, the IVF birth rate is around 20% when the mother is 38 years old and drops to 5% when she reaches 42 years of age.
For this reason, the British institute recommends performing at least 3 IVF cycles before considering a change in strategy.
4. Is in vitro fertilization safe for mother and baby?
IVF is a procedure that’s safe enough to be carried out in the event of the desire to achieve motherhood.
Regarding maternal health, hypotheses have been postulated about the risk of breast, ovarian, and endometrial cancer as a consequence of the high levels of estrogens received for the stimulation of ovulation. However, the lack of prospective and well-designed clinical trials to date makes it impossible to assert this.
As for the baby, the evidence about the risk of suffering from some future health condition is heterogeneous and quite controversial.
Some population studies have shown that these youngsters have a slightly increased risk of genetic disorders when compared to naturally conceived children. But this could also be linked to maternal lack of fertility, so more specific studies are required to establish a causal relationship.
5. Can genetic defects be detected in embryos before implantation?
There is a genetic defect screening technique that can be carried out in embryos before they’re implanted. The goal is to avoid implanting an egg with an abnormal number of chromosomes (aneuploidy), but not to diagnose any specific health condition.
In fact, this technique is reserved for those couples who are at increased risk of conceiving a child with this type of genetic disorder. For example, advanced maternal age (from 35 years) or history of repeated miscarriages, although the latter condition is disputed.
6. Will I have twins if I opt for in vitro fertilization?
At present, advanced techniques are available that allow the implantation of fewer embryos, but of higher quality. This allows a woman to carry out a single pregnancy (of one embryo) and come to term normally.
In cases where more than one egg is to be implanted, the recommended maximum is 4 embryos per IVF cycle, depending on maternal age.
7. What happens to non-implanted embryos?
Embryos that aren’t implanted can be reserved for different purposes:
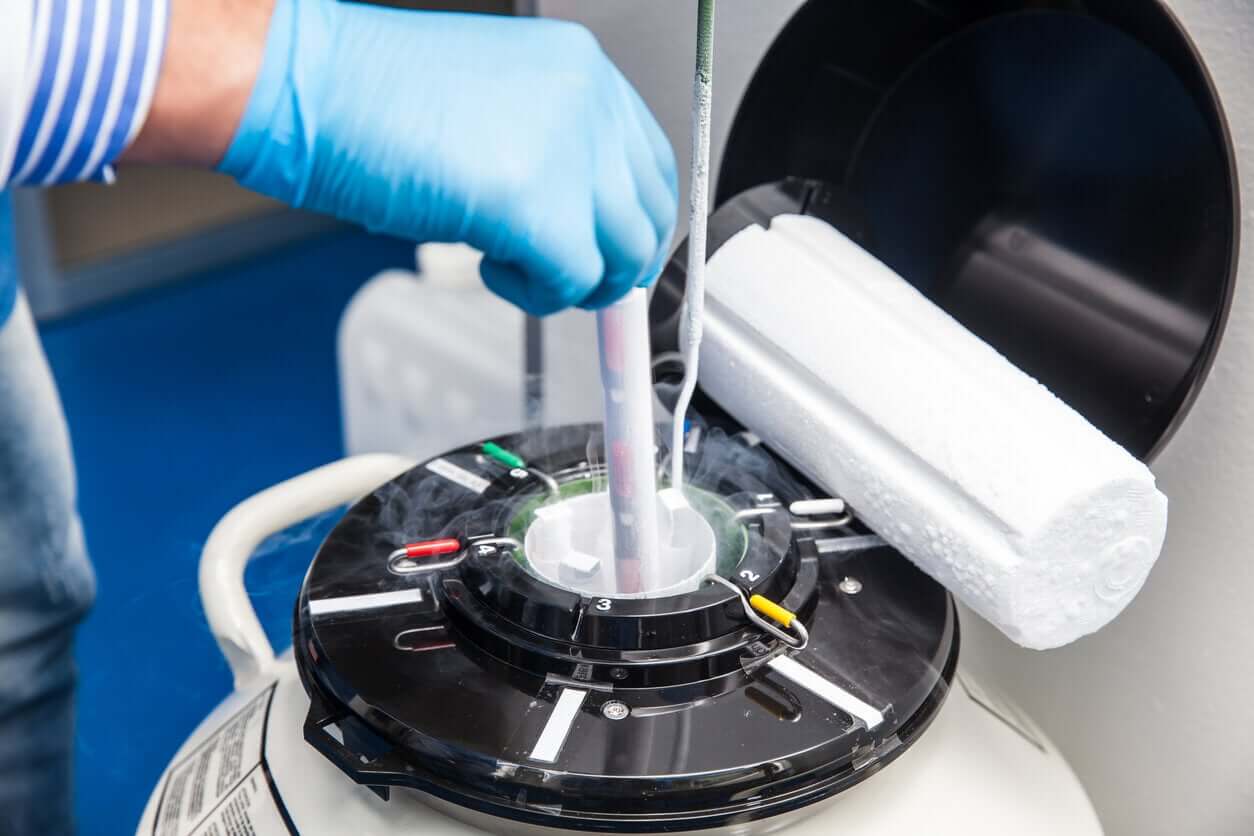
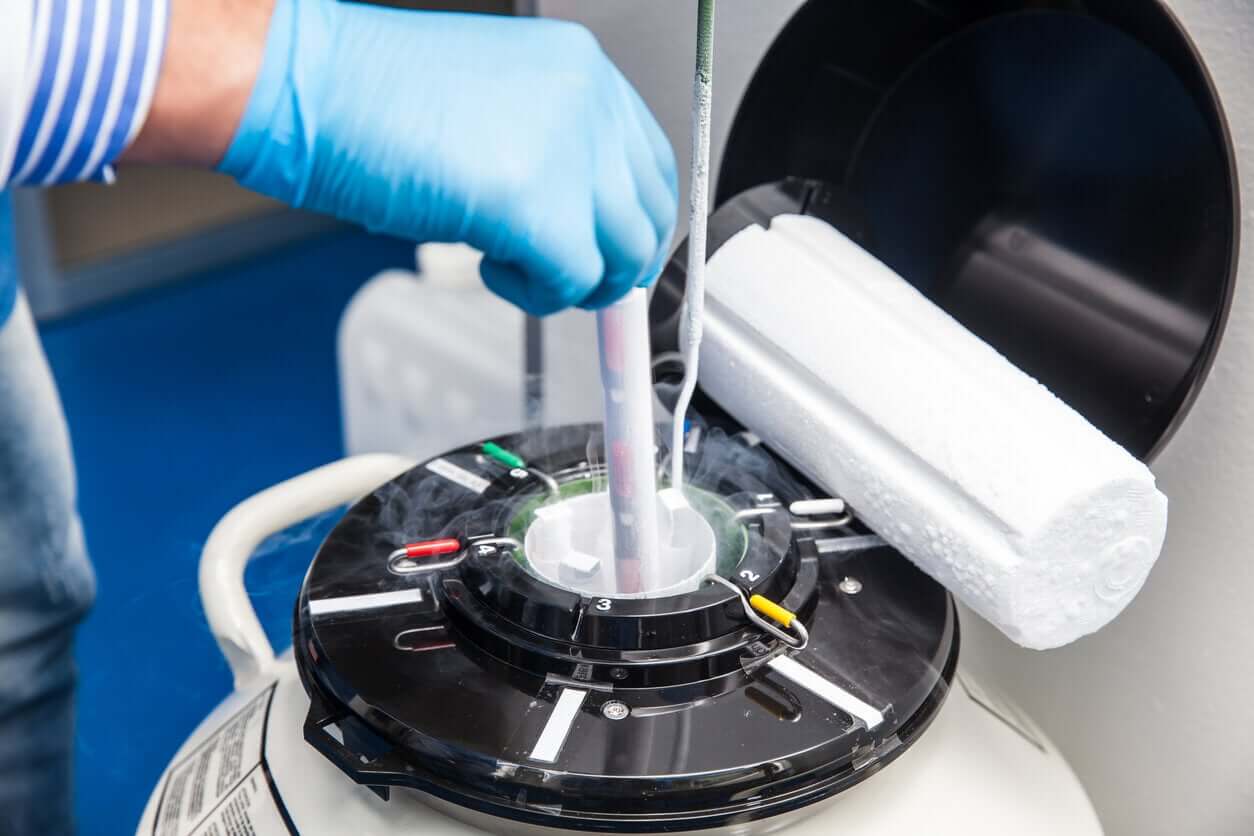
- Cryopreservation for a future implantation.
- Donation for reproductive purposes.
- Donation for research in reproductive medicine to specialized centers.
All the alternatives described require the consent of the parent(s) and this consent must be renewed from time to time. After the period established by law for the conservation of the eggs, the process ceases.
8. I don’t have a partner but I want to be a mother, is it possible to access fertilization with a donor?
Of course, and the assisted reproduction law that governs the United States endorses the confidential donation of gametes (oocytes or sperm) or pre-embryos. Therefore, in the case of a single mother or single-parent families, this option is valid for conceiving a child.
9. Is there an age limit for IVF?
Generally speaking, there’s no legal or ethical limit to motherhood. However, scientific societies recommend not seeking pregnancy at very advanced ages, as this increases the risk of illnesses of pregnancy. For example, pre-eclampsia, gestational diabetes, or placental problems.
Therefore, the Spanish Fertility Society advises against the use of IVF in women over 50 years of age.
Don’t give up on your dream of being a mom!
As you can see, motherhood can be possible through IVF. If you’re ready to try it, consult the specialized centers in your city and start making your dream of being a mother come true.
Since the 1970s, the conception of a child outside the womb has been a reality. In fact, its frequency is such that we’ve already lost sight of the magnitude of the astonishing discovery of Robert Edwards and his colleagues. Today, millions of children come to the world thanks to advances in reproductive medicine. It’s estimated that between 1 and 3% of live births in Europe and the United States were conceived by in vitro fertilization (IVF). The dream of being a parent can come true and that’s why today, we want to answer the 9 most frequently asked questions about in vitro fertilization!
In vitro fertilization, 40 years fulfilling dreams
In 1978, Louise Brown, the first “test-tube baby”, conceived in the laboratory by IVF, came to this world. From there, for many families, the story began to change and their dream of being parents came true.
We know that any promising alternative brings with it fears and doubts, and that’s why we’re going to answer the most frequent questions about in vitro fertilization that arise among families. With information, it’s possible to make more conscious and wise decisions.

1. What is the in vitro fertilization technique?
IVF is a highly complex assisted fertilization (AF) technique, which specifies three fundamental steps of reproduction :
- Obtaining the mature oocyte (maternal gamete), from the aspiration of the pre-ovulatory follicle of the woman’s ovary.
- The fertilization of the oocyte by the sperm (paternal gamete): this gives rise to the egg or embryo.
- The transfer of the embryo into the uterine cavity, to complete its gestation.
This way, reproductive medicine specialists are in charge of executing a key step for the creation of life when it’s not possible to do it naturally.
2. When should couples consider this option?
AF techniques, especially IVF, are effective alternatives to conceiving a baby in those cases where there are difficulties in achieving it. And these can be medical issues, such as infertility, or social issues, such as single-parent families.
The most important thing is to consult a specialist in assisted reproduction so that they can evaluate each case in particular and suggest the most appropriate method.
3. How likely is this technique to be successful?
In general, the chances of conceiving naturally are around 20% in a young, healthy couple. But in medicine, the question isn’t mathematical. In fact, with successive attempts, this percentage drops month by month.
In the case of IVF, the success rate depends on many factors, including maternal age. According to data from the National Institute of Health and Care Excellence in the United Kingdom, the IVF birth rate is around 20% when the mother is 38 years old and drops to 5% when she reaches 42 years of age.
For this reason, the British institute recommends performing at least 3 IVF cycles before considering a change in strategy.
4. Is in vitro fertilization safe for mother and baby?
IVF is a procedure that’s safe enough to be carried out in the event of the desire to achieve motherhood.
Regarding maternal health, hypotheses have been postulated about the risk of breast, ovarian, and endometrial cancer as a consequence of the high levels of estrogens received for the stimulation of ovulation. However, the lack of prospective and well-designed clinical trials to date makes it impossible to assert this.
As for the baby, the evidence about the risk of suffering from some future health condition is heterogeneous and quite controversial.
Some population studies have shown that these youngsters have a slightly increased risk of genetic disorders when compared to naturally conceived children. But this could also be linked to maternal lack of fertility, so more specific studies are required to establish a causal relationship.
5. Can genetic defects be detected in embryos before implantation?
There is a genetic defect screening technique that can be carried out in embryos before they’re implanted. The goal is to avoid implanting an egg with an abnormal number of chromosomes (aneuploidy), but not to diagnose any specific health condition.
In fact, this technique is reserved for those couples who are at increased risk of conceiving a child with this type of genetic disorder. For example, advanced maternal age (from 35 years) or history of repeated miscarriages, although the latter condition is disputed.
6. Will I have twins if I opt for in vitro fertilization?
At present, advanced techniques are available that allow the implantation of fewer embryos, but of higher quality. This allows a woman to carry out a single pregnancy (of one embryo) and come to term normally.
In cases where more than one egg is to be implanted, the recommended maximum is 4 embryos per IVF cycle, depending on maternal age.
7. What happens to non-implanted embryos?
Embryos that aren’t implanted can be reserved for different purposes:
- Cryopreservation for a future implantation.
- Donation for reproductive purposes.
- Donation for research in reproductive medicine to specialized centers.
All the alternatives described require the consent of the parent(s) and this consent must be renewed from time to time. After the period established by law for the conservation of the eggs, the process ceases.
8. I don’t have a partner but I want to be a mother, is it possible to access fertilization with a donor?
Of course, and the assisted reproduction law that governs the United States endorses the confidential donation of gametes (oocytes or sperm) or pre-embryos. Therefore, in the case of a single mother or single-parent families, this option is valid for conceiving a child.
9. Is there an age limit for IVF?
Generally speaking, there’s no legal or ethical limit to motherhood. However, scientific societies recommend not seeking pregnancy at very advanced ages, as this increases the risk of illnesses of pregnancy. For example, pre-eclampsia, gestational diabetes, or placental problems.
Therefore, the Spanish Fertility Society advises against the use of IVF in women over 50 years of age.
Don’t give up on your dream of being a mom!
As you can see, motherhood can be possible through IVF. If you’re ready to try it, consult the specialized centers in your city and start making your dream of being a mother come true.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Ginsburg E, Racowsky C. In Vitro Fertilization. A Comprehensive Guide. Springer New York Heidelberg Dordrecht London. 2012. ISBN: 978-1-4939-4217-6
- Bruna Catalán I, Coroleu Lletget B. Lo esencial en medicina reproductiva. Elsevier España. 2016. ISBN: 978-84-9113-098-7
- Eskew AM, Jungheim ES. A History of Developments to Improve in vitro Fertilization. Mo Med. 2017 May-Jun;114(3):156-159. PMID: 30228571; PMCID: PMC6140213. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140213/
- Fishel S. First in vitro fertilization baby-this is how it happened. Fertil Steril. 2018 Jul 1;110(1):5-11. doi: 10.1016/j.fertnstert.2018.03.008. Epub 2018 Jun 13. PMID: 29908772. Disponible en: https://pubmed.ncbi.nlm.nih.gov/29908772/
- Society for Assisted Reproductive Technology website. Frequently asked questions. [Internet] https://www.sart.org/patients/frequently-asked-questions/
- National Institute for Health and Care Exelence website. The importance of 3 full cycles of IVF. 2014. [Internet] https://www.nice.org.uk/news/blog/the-importance-of-3-full-cycles-of-ivf
- Ethics Committee of the American Society for Reproductive Medicine: Oocyte or embryo donation to women of advanced age: a committee opinion. Fertil Steril. 2013; 100: pp. 337-340.
- Carolan M: Maternal age>/=45 years and maternal and perinatal outcomes: a review of the evidence. Midwifery 2012; 29: pp. 479-489. Disponible en: https://pubmed.ncbi.nlm.nih.gov/23159159/
- Brinton LA, Scoccia B, Moghissi KS, Westhoff CL, Niwa S, Ruggieri D, et. al.: Long-term relationship of ovulation-stimulating drugs to breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2014; 23: pp. 584-593. Disponible en: https://pubmed.ncbi.nlm.nih.gov/24700523/
- Hansen M: Assisted reproductive technology and birth defects: a systematic review and meta-analysis. Hum Reprod. 2013; 19: pp. 330-353. Disponible en: https://pubmed.ncbi.nlm.nih.gov/23449641/
- Ley 14/2006, de 26 de mayo, sobre técnicas de reproducción humana asistida. Disponible en: https://www.boe.es/buscar/act.php?id=BOE-A-2006-9292
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








